Here we cover some bits and bobs about drugs that we wish we knew and understood a little better as a junior doctor…hopefully you’ll find these tips helpful…..
We will cover: ‘top tips on bowel prep‘, ‘interstitial nephritis…more common than you realise‘, ‘a note on nephrotoxins‘, ‘why aren’t ACEi/ARBs nephrotoxins then?‘, ‘why aren’t diuretics nephrotoxins..they can make the sCr worse though, can’t they?‘, ‘common questions about CKD drugs‘ and ‘herbal meds and recreational drugs…are they bad for the kidneys?‘
Top Tips on Bowel Prep!
- First…check your local hospital protocol but here are some principles…. [1-4]
- In colonoscopy, is bowel preparation necessary and appropriate?
- An alternative to colonoscopy is CT colonography with faecal tagging (does not require prep)
- All patients must have a U+E check within 6 weeks of receiving bowel prep
- Sodium phosphate containing agents are contraindicated in CKD
- Patients with heart failure should suspend their diuretics on the day of procedure and for the 1st 48 hours
- ACEi/ARBs can be continued at the discretion of the endoscopist
- Check all CKD stage 5 (eGFR <15) patients with a nephrologist
- All CKD stage 5 patients are recommended to have elective admission
- All CKD stage 5 patients must have their U+Es checked 24 hours post-procedure – if sCr rises by 30% or more, serum K <3.0 or >6.5, serum Na <130 or >150 – discuss with the renal team
- CKD 1-3 (eGFR >30) and renal transplant (eGFR >30) acceptable agents:
- Klean Prep
- Movi Prep
- Picolax
- Citrafleet
- Chronic haemodialysis and peritoneal dialysis acceptable agents:
- Picolax
- Citramag
- CKD stage 4 (eGFR 15-30) acceptable agents:
- Moviprep (if able to tolerate larger fluid volumes)
- Picolax/Citramag/Citrafleet (if risk of volume overload)
- CKD stage 5 (eGFR <15) acceptable agents:
- Picolax
- Citrafleet
- Citramag
Interstitial Nephritis…more common than you realise!
- We see this a lot (it’s more common that you probably think…!) and can cause an AKI severe enough to need acute dialysis (in some cases it can also cause rash, eosinophilia and low-grade temperatures) [5]
- Also termed tubulointerstitial nephritis or acute interstitial nephritic
- Caused by inflammation (acute or chronic) of the renal tubulointerstitium usually mediated by a ‘hypersensitivity’ reaction to drugs (in rare cases it can be due to inflammatory or autoimmune diseases such as sarcoidosis, IgG4 disease, Sjogrens…)
- >250 medications are known to cause this reaction
- Common meds include:
- Beta-lactam and fluouroqinolone antibiotics
- PPIs
- NSAIDs
- Chemotherapy/Immunotherapy agents
- Also caused by infections, some cancers and TINU syndrome (tubulo-interstitial nephritis with uveitis)
- If suspected or confirmed…the patient should avoid the offending medication in future
- Diagnosis is made on renal biopsy but if you suspect this then stop the probable offending drug and the kidney function might improve. Steroids can help kidney function recover further but not in all cases. If you suspect this diagnosis…involve the renal team!
A note about ‘Nephrotoxins’….
- We often see the term ‘nephrotoxins’ written in patient notes and…whilst very important to suspend in AKI…we frequently see medications that are not actually nephrotoxins stopped but not restarted and this…in some cases….can have adverse effects on the patient… [6]
- What drugs are often labelled as nephrotoxins but are NOT…
- ACEi /ARBs
- Diuretics
- What are GENUINE nephrotoxins (drugs which acutally cause direct damage to the kidney where risks of the drug may outweigh the benefits to the patient…
- Aminoglycosides (e.g. gentamycin)
- Iodinated contrast
- Some chemotherapies e.g. cisplatin
Why aren’t ACEi/ARBs ‘nephrotoxins’ then…?
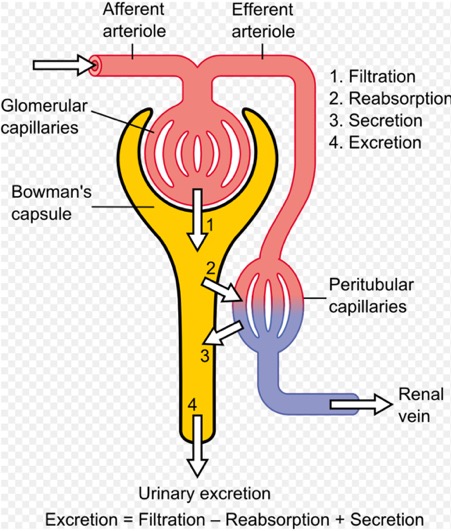
- They are not ‘nephrotoxins’ as they do not cause kidney damage – they, in fact, concentrate blood flow to the kidney tubules which are an area very sensitive to hypoxia [7]
- It is normal for these drugs to cause an acute reduction in GFR once commenced due to altered glomerular haemodynamics caused by renal efferent arteriole relaxation
- Acute increases of sCr of up to 30% are normal in the first 2 months of treatment (only discontinue if rise exceeds this)
- ACEi/ARBs are extremely beneficial in patients with HFrEF and they slow the progression of proteinuric kidney disease – this is done by reducing glomerular perfusion and haemofiltration
- Temporary cessation of these drugs is unlikely to cause harm BUT they must be re-introduced as soon as clinically possible to avoid other potential harm from their absence
- Various trials/post-hoc analyses show that continuation of ACEi/ARBs have a favourable impact on mortality even when renal function is worsening compared to patients without worsening renal function AND acute pulmonary oedema was one of the commonest causes of admission to hospital after an episode of AKI possibly due to inappropriate withdrawal of ACEi/ARBs and diuretics
- Every discontinuation MUST also come with instructions as to when safe for re-initiation of the drug
- They should not be continued in hyperkalaemia or hypovolaemia/sepsis as thought to exacerbate pre-renal AKI and hyperkalaemia
Why aren’t diuretics ‘nephrotoxins’…they can make the sCr worse can’t they!?!
- For the majority of patients with HF, diuretics are essential [9]
- As HF progresses, worsening renal function in the setting of aggressive diuretic administration reflects a haemodynamic change in GFR, not direct renal injury
- In HF where high doses of diuretics are needed for fluid retention, a decline in renal function is not an indication to reduce diuretic dose…in fact, if the patient remains congested then more diuretics are required
- Remember…CKD and AKI are powerful prognostic markers for both kidney disease AND cardiovascular disease – even small sCr rises during treatment of HF indicate a poorer prognosis and a ‘higher risk’ patient group
- As for ACEi/ARBs…evidence suggests that stopping diuretics during AKI or worsening CKD results in increased likelihood of readmission/admission to hospital with pulmonary oedema
- BUT diuretics should be withheld if the patient is hypovolaemic as offloading more fluid in this situation will cause pre-renal AKI
Common questions about CKD drugs…
- If a patient with CKD or on renal replacement therapy (PD/HD) are on your ward, you may notice some unfamiliar drugs they are on
- We often get called about whether to stop, start or increase these drugs in inpatients and we’re always happy to help with this
- Most of the time, this is taken care of in renal clinic but here are a few important tips about each of the four main CKD drugs…
- EPO (erythropoietin) [10]
- Boosts haemoglobin, improves quality of life by treating symptomatic anaemia in patients and reduces need for blood transfusions
- Most CKD stage 5/RRT patients are on these (when Hb falls below 10g/dL)
- Remember to check for other causes of anaemia first and correct and once you have done this…the patient may need to have epo started/their dose increased (contact the renal team to organise)
- Cannot be given in severe hypertension as increases stroke risk, should be stopped immediately if Hb is too high as stroke risk is increased, contra-indicated in certain malignancies as overall survival is reduced and tumour progression/recurrence is increased (breast, non-small cell lung, head and neck, lymphoid and cervical cancers and certain cancer treatments)
- Phosphate binders
- If a CKD patient’s phosphate is high, ensure they are on a low phosphate diet (ask the dieticians to review)
- Phosphate binders are indicated in secondary and tertiary hyperparathyroidism….most patients with advanced CKD have this
- To check for secondary hyperparathyroidism – check calcium, phosphate and PTH (and vitamin D level)…once you have checked these – contact the renal team for advice if any of these parameters are out of range
- Common phosphate binders include calcium acetate, calcium carbonate, sevelemer hydrochloride and lanthanum carbonate
- The reason to treat CKD-related hyperparathyroidism is to reduce complications such as renal bone disease, complications from hypercalcaemia, itch, soft-tissue calcification/breakdown and poor wound healing
- Vitamin D analogues
- Common analogues are colecalciferol, alfacalcidol and paracacitol
- Also used to treat and prevent secondary and tertiary hyperparathyroisim (see phosphate binders above…)
- Cinacalcet
- This is a calcimimetic (mimics hypercalcaemia) which directly lowers PTH in hyperparathyroidism by increasing the sensitivity of the calcium sensing receptor to extracellular calcium
- This drug can be dangerous so can only be prescribed by consultant nephrologists
- Quite a few patients with advanced CKD/RRT take this drug
- It can rapidly lower calcium so remember to stop this drug and contact the renal team if you see a patient on it with severe hypocalcaemia
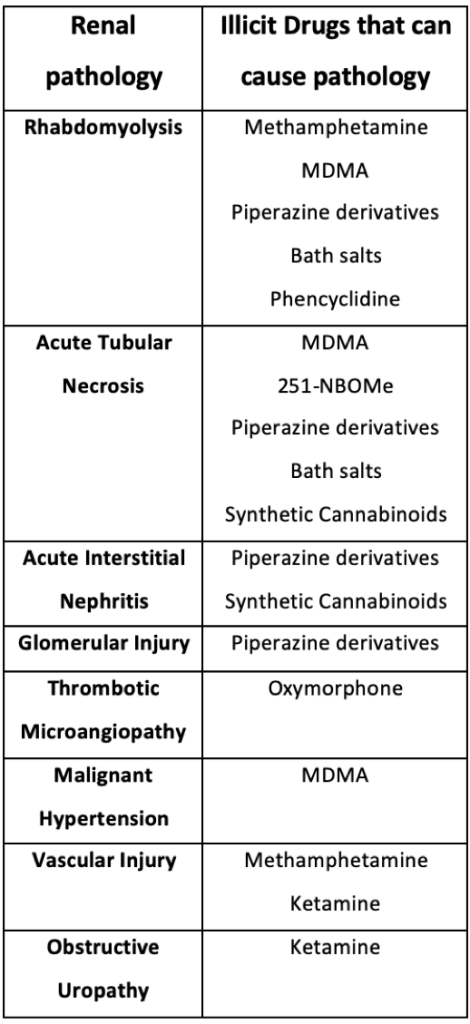
Herbal meds and recreational drugs…are they bad for the kidneys?
- We often see renal consequences of these substances – here’s a summary of renal pathologies that can occur
- Basically…if you see AKI in a patient who has taken illicit drugs/herbal medicines…check for the obvious things such as rhabdomyolysis and then call the renal team if otherwise not clear…
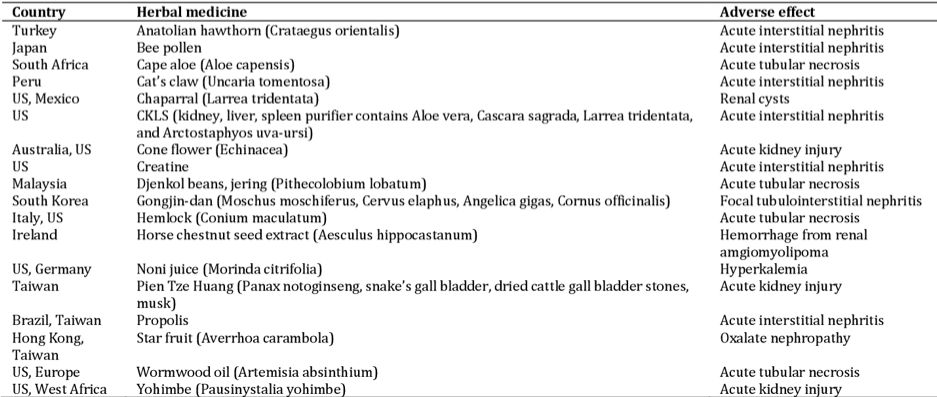
- Some Ayurvedic medicines contain heavy metals which can cause renal impairment
- Some Chinese herbal medicines can cause renal impairment when used in combination with conventional medicines
- Herbal preparations containing Aristocholic acid can cause Acute interstitial nephritis
- St John’s Wort and other herbal medicine can potentiate the effects of Ciclosporin and Tacrolimus which are used in renal transplant patients causing AKI, hyperkalaemia and other non-renal effects
- Acute oxalate nephropathy can be seen every so often from ethylene glycol ingestion (anti-freeze), ascorbic acid and large quantities of iced tea consumption and ‘green smoothie cleanses’
There are many pitfalls and tricks to dealing with drugs in renal transplant patients…we will cover these tips in ‘Tales of a Transplant Patient – clinical pearls and pitfalls!’
References
- Hartmann, B. et al. Drug Therapy in Patients with Chronic Renal Failure. Dtsch Arztebl Int (2010). 107(37): 647-656.
- Gallieni, M., Cancarini, G. Drugs in the elderly with chronic kidney disease: beware of potentially inappropriate medications. Neph Dial Transpl (2014). 30(3): 342-344.
- Guidelines for Medicine Optimisation in Patient with Acute Kidney Injury ‘Think Kidneys’ (2016): https://www.thinkkidneys.nhs.uk/aki/wp-content/uploads/sites/2/2016/03/Guidelines-for-Medicines-optimisation-in-patients-with-AKI-final.pdf
- Consensus Guidelines for the Safe Prescription and Administration of Oral Bowel Cleansing Agents. The Renal Association: https://renal.org/wp-content/uploads/2017/06/Consensus_guidelines_for_the_prescription_and_administration_of_oral_bowel_cleansing_agents_January_2011-1.pdf
- Praga, M. Gonzalez, E. Acute Interstitial Nephritis. Kid Int (2010). 77(11): 956-961.
- Jones, M., Tomson, C. Acute kidney injury and ‘nephrotoxins’: you’re your language. Clin Med (Lond)(2018). 18(5): 384-386.
- Tomson, C., Tomlinson, L. A. Stopping RAS Inhibitors to Minimize AKI. More Harm than Good? CJASN(2019). 14(4): 617-619.
- https://commons.wikimedia.org/wiki/File:Physiology_of_Nephron.png
- Tomson, C. Blakeman, T. Treat the person, not the test result: New guidelines on changes in kidney function during treatment of heart failure. Royal College of General Practitioners (2019): https://www.rcgp.org.uk/clinical-and-research/about/clinical-news/2019/june/new-guidelines-on-changes-in-kidney-function-during-treatment-of-heart-failure.aspx
- Kei, T. et al. Efficacy and safety of erythropoietin and iron therapy to reduce red blood cell transfusion in surgical patients: a systematic review and meta-analysis. Can J Anaesth (2019). 66(6): 716-731.
- Tangkiatkumjai, M. Existing evidence for safe use of herbal medicines in chronic kidney disease. Int J Pharm Pharm Sci (2015). 7(9).
- Luciano, R. L., Perazella, M. A. Nephrotoxic effects of designer drugs: synthetic is not better! Nat Rev Nephrol (2014): 10(6): 314-324.
