Haemodialysis patients get more than their fair share of medical problems requiring hospitalisation or intervention. Each problem can easily be manged by the appropriate team, however here we will outline some special considerations tailored to the HD patient to add to your tool kit!
Acute Coronary Syndrome
- ACS is common amongst renal patients and they have a worse outcome compared to those without CKD [1]
- Chest pain can be caused by all the normal things in renal patients but have the increased risk of ACS in your mind as well as uraemic pericarditis and arrhythmias which are more common (and air embolismfrom HD/access…but this is rare)
- What about ECGs?
- Can be difficult to interpret due to LVH, BBB and changes related to high K+
- Prolonged QTc intervals are more common than the general population, as are arrhythmias [2]
- Troponins are chronically elevated in ESRF and HD will reduce the blood concentration of highly sensitive cardiac troponins – so focus on the TREND (rather than isolated readings) and keep the effects of HD on trop in mind! [3]
- Patients who have had ACS usually need adjustment to their dialysis prescription shortly afterwards to avoid rapid electrolyte shifts and fluid removal that may be more likely to precipitate arrhythmias post-MI. Let the renal team know of any ACS as we would prefer to give more frequent HD, more slowly and cautiously early after MIs (if we can!)
- If an angiogram is required we may want to dialyse the patient afterwards – if a large amount of fluid/contrast is given then we may wish to do this to avoid pulmonary oedema (if the patient is sensitive to this). If a patient has some residual renal function then we may want to try to preserve this by providing HD after contrast too – so let us know of this
- What about ACS drugs?
- Aspirin – no changes necessary usually
- Beta-blockade – we don’t know which is the best beta-blocker to use (clinical trials ongoing) but Carvedilol is the least dialysed [4]. Avoid if intra-dialytic hypotension related to bradycardia. Hyperkalaemia can occur so cautiously increase the dose and monitor K+ (ideally on HD) as titrating
- ACE inhibitors – can cause hyperkalaemia so cautiously increase dose and monitor K (ideally on HD) as titrating up
- Clopidogrel – no dose adjustment required (although HD patients usually excluded from trials)
- Ticagrelor – no dose adjustment required. Use not recommended in ESRF population due to lack of data [5]
- Prasugrel – no dose adjustment required. Drug labels remind of very limited experience in HD patients [5]
- Low Molecular Weight Heparins – all types need to have drug level monitoring and dose adjustment. High doses can cause hyperkalaemia so monitor K+ and cautiously adjust dose
- Glycoprotein IIb/IIIa Receptor Inhibitors – contraindicated at different levels of GFR and different instructions for each drug [6] (Abciximab/Eptifibatide/Tirofiban) – consult with the renal drug database, drug SPC and your clinical pharmacist
- Statins – no trial data in ESRF WITH ACS. Some smaller studies show improved mortality [7]. Same monitoring needed – CK and LFTs (rhabdomyolysis can cause hyperkalaemia in HD patients if occurs)
Infection
- There are a few extra sources of infection to consider in HD patients:
- Line infections
- AV grafts
- AV fistulas can become infected mainly after recent creation
- Bladder (if anuric/oliguric the bladder can fill up with pus without anyone realising) – a quick aseptic in-out catheter can diagnose this
- Endocarditis (is more common often due to infected neck lines)
- Osteomyelitis and septic arthritis (is also more common due to seeding from lines)
- Opportunistic infections (as many patients are immunosuppressed)
- Atypical presentations of infection are common
- Resistant organisms are common due to frequent antibiotic requirements
- Liaise closely with microbiology as atypical and opportunistic organisms are commonly seen in these patients
- Most antibiotics require a dose adjustment in HD patients (check BNF or renal drug database/handbook)
- Some antibiotics are dialysed so need to be given at the end of dialysis (consult the BNF, your clinical pharmacist or renal team)
- Some antibiotics require level monitoring in HD patients e.g. Vancomycin to avoid the ototoxic consequences (consult the BNF, your clinical pharmacist or renal team)
- If the patient develops an infection that requires protection/source isolation then please let the renal team know so that we can dialyse them in isolation (sometimes this requires time for this to be organised in advance of HD)
- If the patient develops sepsis or septic shock – please let us know as it would typically be unsafe for us to dialyse them in their usual HD unit. Dialysis requires a reasonable blood pressure….if the BP is lower than normal then a more gentle form of dialysis such as CVVH would be usually required in critical care

Bleeding
- The patients HD unit is not the place for a bleeding patient for obvious reasons…so please let us know if this is the case and we can arrange HD in an appropriate place if the patient really needs it (either ITU or in a monitored ward setting)
- We usually need to reduce or withhold the usual anticoagulation that we give on haemodialysis in patients with active or recent bleeding
- If a patient is unstable with bleeding but needs urgent HD (e.g. for hyperkalaemia) then it is usually safer for them to have a more gentle dialysis such as CVVH/CVVHD/SLED on ITU sometimes even with inotropic support
- Blood product transfusions can cause hyperkalaemia (due to haemolysis if excess RBCs when entering the patient) and can risk volume overload so discuss with renal or ITU about how best to deal with this (ideally the patient should be managed on ITU)
- In rare cases – Desmopressin can be considered to help deal with the uraemic platelet dysfunction in HD patients that often worsens major bleeding…but contact the renal team before considering this [10]
DKA
- With diabetic nephropathy being one of the major causes of ESRF in the UK….DKA is not unheard of BUT DKA is actually LESS common in ESRF patients because [11]:
- Reduced kidney gluconeogenesis
- Less insulin clearance (as the kidney doesn’t eliminate it)
- Improved insulin sensitivity
- HD patients are in hospital 3x/week so illness is often detected early
- Because of this…when HD patients develop DKA they usually have a SERIOUS underlying cause (so go looking for this e.g severe infection/ischaemia/pancreatitis etc.)
- Firstly…all the usual DKA protocols (if not specific to HD patients) can be fatal!
- HD patients are at risk of [12]:
- Severe hyperkalaemia (as K excretion reduced)
- Rapid onset hypoglycaemia with treatment (due to delayed renal insulin clearance)
- Increased neurological events (cerebral oedema) due to rapid blood tonicity shifts due as response to insulin is rapid
- Remember, the patient won’t get the massive osmotic diuresis (induced by hyperglycaemia) that is seen in non-renal patients….as a consequence:
- They don’t eliminate K+ as easily (initial high K from hypertonicity, low insulin and acidosis is usually higher in HD patients)
- Often nowhere near as dry (as less able to pass urine and eliminate body water)
- Management of DKA in these patients depends on their fluid status as each responds differently:
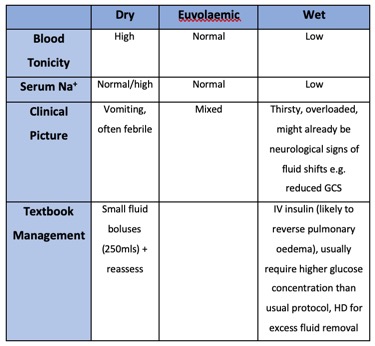
- As HD patients are particularly sensitive to insulin and electrolyte and fluid shifts…
- Ideally should be managed in a critical care setting (get ITU early!)
- Monitor blood glucose very regularly
- Try to avoid insulin boluses (increases hypoglycaemia risk)
- Avoid IV bicarbonate in these patients (risks volume overload and osmolar shift complications)
- If the patient is actually dry – only give small 250mls fluid boluses with frequent fluid status reassessments
- Be very cautious and conservative with K replacement
- Don’t be tempted to dialyse the high K as it won’t fix the cause, it can mask the severity and can worsen fluid shifts resulting in cerebral oedema
Surgical Emergencies and Problems
- There are a few extra things to consider for HD patients undergoing surgery….
- If the patient is unwell or had low BP post-op then please let us know as we may need to dialyse them more cautiously on ITU or in a monitored ward environment
- Let the renal team know in advance of a patients surgery date as we will want to dialyse them pre-operatively and may need to withhold dialysis anticoagulation peri-procedure if the bleeding risk is high
- We are happy to help with post-op analgesia to ensure this is safe as many analgesics can accumulate or be dangerous to HD patients
- Please do not be tempted to give lots of fluid or replace electrolytes in these patients without consulting the renal team as this can often be over-zealous and put the patient at risk of life-threatening hyperkalaemia or overload (mostly this can be addressed by us adjusting the patient’s dialysis script)
- If the patient is having an amputation then we will want to reduce their dialysis target weight based on their new immediate post-op weight so that they don’t become fluid overloaded
- If the patient has a fracture then we will want to reduce or temporarily stop their dialysis anticoagulation to avoid bleeding complications
- Imaging with contrast is fine but if the patient has some residual renal function that we wish to preserve or if they are very sensitive to volume overload then we would usually wish to dialyse them after the contrast load (it is likely that they have some residual renal function if they are not completely anuric)

Head Injury and Stroke
- If a patient has had a recent head injury or stroke the please let us know as we would want to withhold their dialysis anticoagulation temporarily or permanently to reduce their bleeding risk
- If the patient is unwell or has a reduced GCS of any degree then the outpatient HD unit will not be the safest or best place for them so please inform us
- In an ischaemic stroke that requires thrombolysis, all the usual thrombolysis cautions are the same…however in renal patients the common absolute contraindications include renal biopsy or dialysis catheter insertion within the last 14 days, uncontrolled hypertension and history of uraemic pericarditis [15]
Calcium Abnormalities
- HD patients can get all the normal causes of low and high calcium but manifestations and complications for hyperparathyroidism are usually the most common
- If calcium is especially low or high then let the renal team know as we may need to adjust their dialysis prescription so we don’t make things worse
- We deal with secondary and tertiary hyperparathyroidism commonly so can always help with any questions
- One important point…if a patient has had a parathyroidectomy – don’t stop their vitamin D and calcium tablets without discussing with the renal team as this can cause rapid life-threatening hypocalcaemia (also Cinacalcet is a drug that can rapidly lower calcium in patients with tertiary hyperparathyroidism so it’s wise to leave dose adjustments to the renal team)

Pleural Effusions
- Pleural effusions are common in HD patients and are, in most cases, transudative secondary to fluid overload from renal failure
- If an HD patient has a pleural effusion then it is best to let the renal team know as we would want, in most cases, to reduce the patient’s target weight on dialysis to help reduce the effusion size if it’s a transudate secondary to renal failure
- The causes in renal patients don’t differ to the typical causes of pleural effusion in other patients so don’t assume it is due to renal failure as you may miss something more serious
- If you plan to perform pleural aspiration then let the renal team know as we will want to do a couple of things:
- Plan HD around the procedure so that the two don’t clash
- Withhold normal dialysis anticoagulation peri-procedure so bleeding risk is reduced
- If aspiration of a lot of fluid is done then we will want to drop the patients dialysis target weight by this volume so that the fluid removed doesn’t reaccumulate
Ascites
- The causes of ascites in renal patients doesn’t differ to the causes in other patients, however a transudate (usually from renal failure) is more common
- Don’t assume that the ascites is due to renal failure as you may miss a serious cause
- If you plan to drain a HD patient’s ascites then let the renal team know as we will want to do a couple of things:
- Reduce the patient’s HD target weight by the amount of fluid drained so that the volume drained does not reaccumulate
- Plan HD around the procedure so that the two don’t clash (please don’t send the patient to their normal dialysis session/unit with an ascitic drain in situ as this would be dangerous – discuss with us before you do the procedure)
- Withhold normal dialysis anticoagulation (if necessary) peri-procedure so bleeding risk is reduced
References
- Santopinto, J.J. et al. Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE). Heart, 2003. 89: 1003-1008.
- Matsumoto, Y. et al. Changes in QTc interval in long-term haemodialysis patients. PLoS One, 2019. 14(1): e0209297.
- Jain, N., Hedayati, S. S. How should clinicians interpret cardiac troponin values in patients with ESRD? Semin Dial, 2011. 24(4): 398-400.
- Vangala, C., Winkelmayer, W.C. Heterogeneity in Outcomes Among Beta-Blockers Elucidated by Intradialytic Data. AJKD, 2018. 72(3): 318-321.
- Summaria, F. et al. Antiplatelet Therapy in Haemodialysis Patients Undergoing Percutaneous Coronary Interventions. Nephrourol Mon, 2015. 7(4): e28099.
- Khaja, A. et al. Percutaneous coronary intervention and the use of glycoprotein IIb/IIIa inhibitors in patients with chronic kidney disease on dialysis: a single centre experience. Haemodial Int, 2008. 12: 2-8.
- Wanner, C. et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing haemodialysis. N Engl J Med, 2005. 353: 238-248.
- https://commons.wikimedia.org/wiki/File:Blausen_0153_CABG_Double.png
- https://commons.wikimedia.org/wiki/File:Hickman_line_catheter_with_2_lumens.jpg
- Hedges, S.J. et al. Evidence-based treatment recommendations for uraemia bleeding. Nat Clin Pract Nephrol, 2007. 3(3): 138-153.
- Tzamaloukas, A.H., et al. Body fluid abnormalities in severe hyperglycaemia in patients on chronic dialysis: review of published reports. J Diabetes Complicat, 2008. 22(1): 29-37.
- Schaapveld-Davis, C.M. et al. End stage renal disease increases rates of adverse glucose events when treating diabetic ketoacidosis or hyperosmolar hyperglycaemic state. Clin Diabetes, 2017. 35(4): 202-208.
- Kaldany, A. et al. Reversible acute pulmonary oedema due to uncontrolled hyperglycaemia in diabetic individuals with renal failure. Diabetes Care, 1982. 5(5): 506-511.
- https://commons.wikimedia.org/wiki/File:CT_of_a_normal_abdomen_and_pelvis,_axial_plane_44.png
- NICE Guidance for Stroke and Transient Ischaemic Attack in over 16s [www.nice.org.uk]
