Hopefully these ‘top tips’ will help you know how and when we can help and how to be perfectly prepared for all the questions we will ask you over the phone….Here we will go over phone/urgent referral criteria, indications for dialysis, how to perfect our ‘dream’ renal referral, tips on transferring renal patients, AKI – what not to miss, should they have dialysis..?, who we want to see in clinic and some key points…!
Referral Criteria (who to refer over the phone)… [1]
- All patients who require urgent renal replacement therapy (i.e. dialysis) – see below for dialysis indications…
- Stage 3 AKI
- Patients admitted with stage 4 or 5 CKD (eGFR <30)
- Patients with complications associated with AKI
- Renal transplant patients
- Any renal patients receiving immunosuppression
- Patients with inadequate response to treatment
- Patients with an unexplained cause of AKI (regardless of stage)
- Patients with possible diagnosis that may need specialist treatment e.g. glomerulonephritis, vasculitis, interstitial nephritis, myeloma
Dialysis Indications (reminder)
A – acidosis (make sure this is a renal acidosis by checking lactate, ketones and anion gap)
E – electrolyte abnormality (hyperkalaemia)
I – ingestions (methanol, ethylene glycol, salicylates etc.)
O – overload (fluid overload)
U – uraemic pericarditis or encephalopathy (check for a pericardial rub, and ECG for ST changes….and electrical alterans)
AND those that are unresponsive to standard therapy… (i.e insulin-dextrose and bicarbonate)
Our ideal referral includes the following info….
- Urine dip result
- Fluid status (ideally give us evidence for this i.e. peripheral oedema)
- Serial sCr trends (inclduing baseline sCr)
- Urine output (and input)
- All drugs given recently including over the counter drugs
- Blood pressure results since admission (i.e. lowest and highest)
- Any procedures/contrast given
- Past medical history
Transfer tips
- Don’t transfer a patient without us accepting them first (and we give you the OK to send across..)
- We want to know the following first…serum potassium, pH/bicarb/lactate, full set of observations, GCS
- If they are sick, most trusts also require an ITU review first or the destination hospital’s ITU to be notified of the transfer in case the patient becomes more sick on route
- If they are due to received dialysis or are a dialysis patient – it is important we know what access they have and if it is likely to be working (i.e. AV fistula/dialysis line etc.) and when they were last dialysed
- In general, a transfer would not be deemed safe if the serum K was >6.0 but this would normally need to be discussed with the on call nephrology consultant
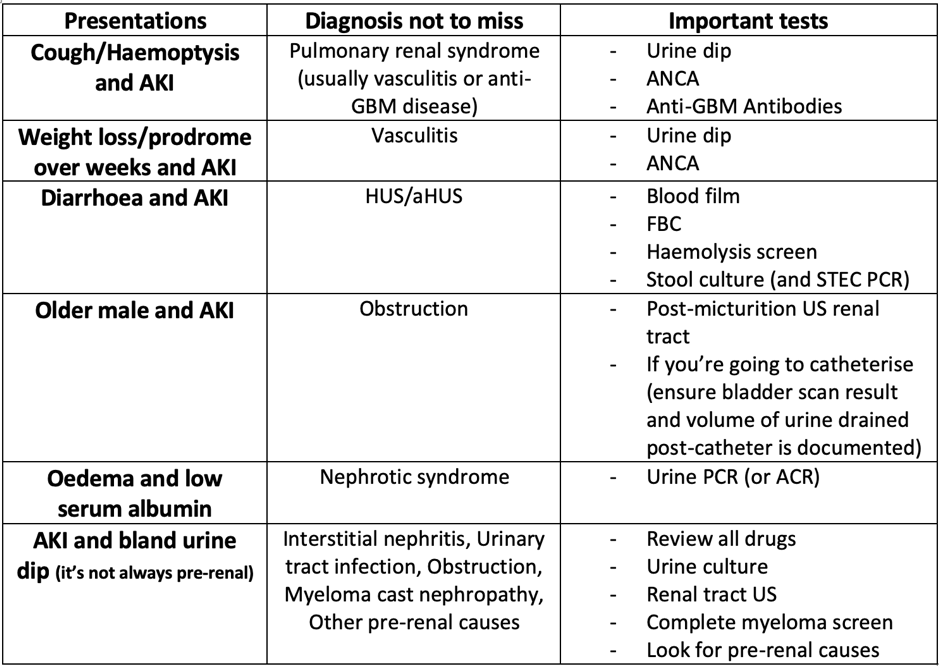
AKI – what not to miss…
But should they have dialysis?
- Dialysis has become more accessible over the years to patients we would have previously not deemed able to have it
- The average age of people when they commence dialysis in the UK is 65 and over 50% have more than one comorbidity [2]
- The prognosis, however, of patients over 80 years old on dialysis is worse than the prognosis of some cancers [3]
- Predicted remaining life expectancy of a patient on dialysis aged 65-69 years is 3.9 years compared to 17.2 years for an aged-matched member of the general population [4]
- All patients that are likely to develop end stage renal failure should receive adequate information about different dialysis treatment modalities including the option of not pursuing treatment (conservative care) [5]
- In the case of AKI, the likelihood of kidney function recovery means that the patient will be more likely to have ‘intermittent dialysis’ until the underlying cause of renal failure is treated or spontaneously recovers (unless the patient declines this treatment or if it is clearly inappropriate for that patient)….this should be approached in much the same way as you would approach a patient requiring level 2 or 3 care in the HDU/ITU setting as dialysis is a form of ‘organ support’
- The survival for patients already established on dialysis who are withdrawing from renal replacement therapy is, on average, 8-10 days (this is very different to those who opt for conservative care) [6]
- Conservative care patients have a variable prognosis (median time often 6 months to 2 years). In fact, for patients over age 75 with poor performance status and high comorbidity scores, dialysis may not actually have a survival benefit over ‘conservative care’ [7, 8]
- Conservative care consists of anaemia treatment, monitoring and addressing fluid balance, treatment of calcium/phosphate to reduce symptoms, advanced care planning and specialist ‘palliative care’. The main aim is to improve quality of life
- This information is important for you as a junior doctor because…
- You may need to make decisions about ‘treatment escalation’ in patients with progressive CKD i.e. are they suitable for CVVH/inotropes/I+V etc. and it is helpful to know their general prognosis
- A CKD patient may be under your care for another reason which may worsen their renal function and decisions about dialysis vs. conservative care may not yet have been made
- You may have to assess the patient’s suitability for another treatment i.e a procedure/surgery and it will be useful to know their prognosis
- In the chronic setting here is some information about prognosis of dialysis in case you are looking after a patient with progressive CKD who is approaching end stage renal failure….
- Consequences of dialysis [9]:
- fatigue/lethargy
- light-headedness/dizziness
- nausea
- headache
- itch
- dry skin
- pain
- muscle cramps
- insomnia
- bone and joint pain
- loss of libido
- erectile dysfunction
- dry mouth
- anxiety and depression
- pill burden
- fluid and diet restrictions
- loss of independence
- In fact, studies have shown that the symptom burden of chronic dialysis is comparable to that of patients with advanced cancer [10]
- The following patient groups, in particular, don’t do as well on dialysis as other patients who receive dialysis treatment [11]:
- Vascular disease
- Diabetes mellitus
- Multiple comorbidities
- Older
- Functionally impaired
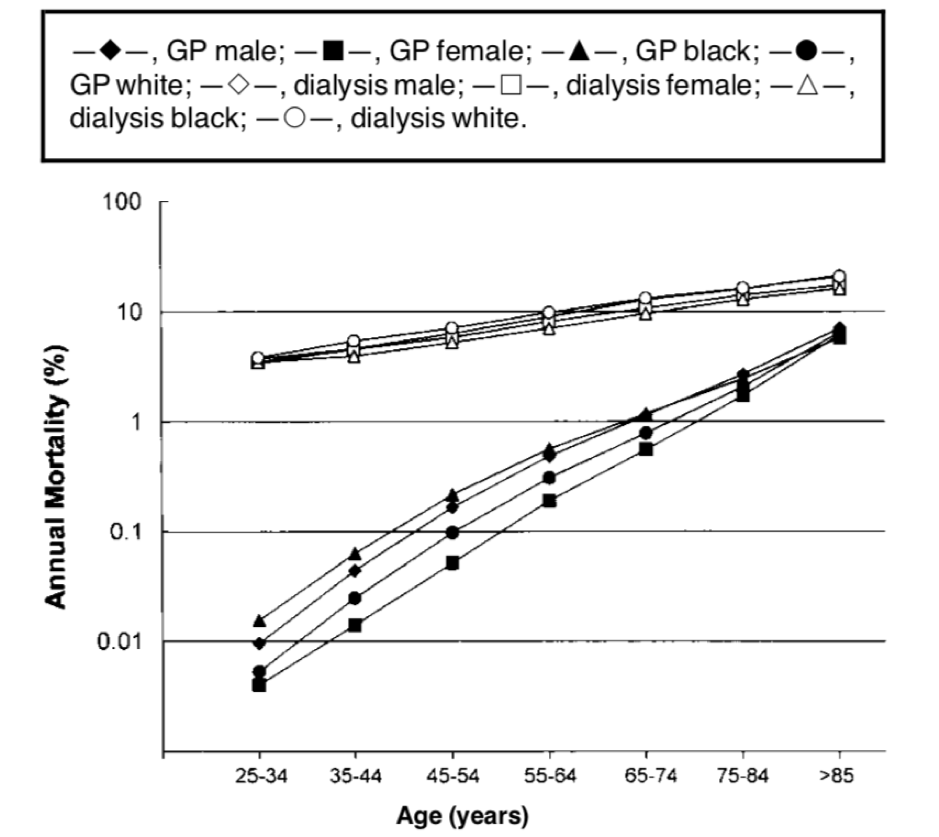
- The following graph is a famous illustration of the poor prognosis of patients receiving dialysis. The bottom line… the mortality risk of a 20 year old person with end stage kidney disease is roughly similar to an 85 year old individual from the general population and was primarily driven by cardiovascular disease…[12]
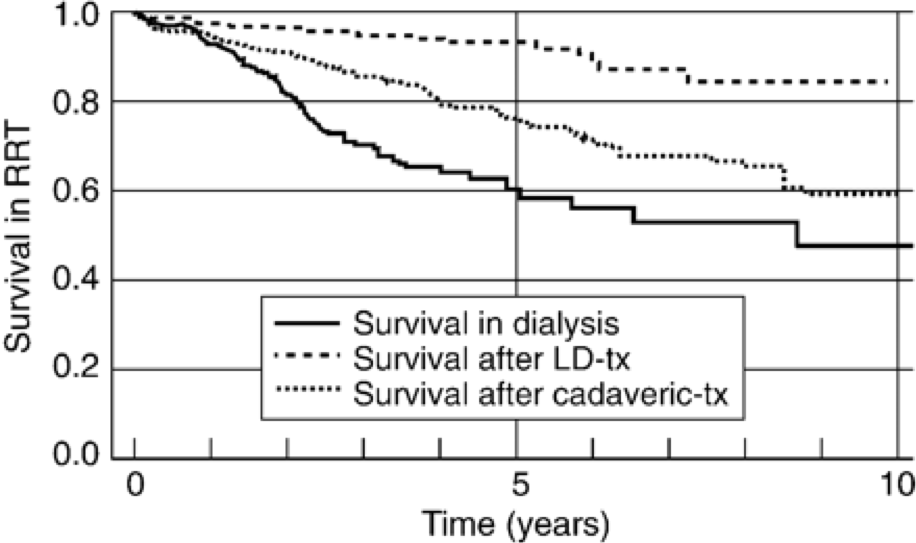
- But it must be noted that survival is dramatically improved when patients get a kidney transplant so it is very important to establish whether the patient is on the transplant list, waiting for a transplant or if they would be a candidate for a transplant in the future….we can advise on this (see below)
Who do we want to see in clinic?
- Nephrotic syndrome (URGENTLY)
- Recent stage 1 or 2 AKI not attributable to sepsis, hypovolaemia or hypotension (URGENTLY)
- CKD stage 4 or above (eGFR <30)
- Sustained decrease in eGFR of >15 or (of >25 if initial eGFR <60) within 12 months
- Urine ACR >70 (unless known to be caused by diabetes and already appropriately treated i.e on maximal tolerated dose of an ACEi/ARB)
- >30% rise in sCr (or >25% eGFR fall) on initiation of up-titration of an ACEi/ARB after excluding alternative causes such as hypovolaemia
- Asymptomatic invisible haematuria in combination with urine ACR >30 mg/mmol irrespective of GFR
- Anaemia (Hb <105 g/l) in CKD stage 3a-5 after excluding other causes of anaemia and after a trial of oral iron (unless if oral iron not tolerated, serum ferritin >100 or transferrin saturations >20%)
- Suspected metabolic stone disease, polycystic kidney disease, renal tubular acidosis or tubulopathy
- Hypertension that is early in onset (age <40) or resistant (BP>140/90 despite maximum tolerated doses of 3 antihypertensives based on the NICE AB/CD algorithm) [1]
Key points
- Call early
- Can it wait until morning?
- Dialysis – is it worth it?
- Acidosis – check with us re. bicarb but check lactate/ketones/anion gap
- Hyperkalaemia – remember insulin-dextrose is a K+ hiding therapy so call us if the underlying cause not clear
- Be confident with your fluid status and go for it (lungs are more important than kidneys)
- Multi-organ failure/unsafe to transfer/haemodynamic instability – call ITU
- Don’t send haemodialysis patients to their usual haemodialysis unit if they’re sick (call us first…)
- Let us know if they’re ours and they’re in (mainly transplant, CKD stage 4/5, dialysis, renal patients taking immunosuppression)
References
- The Renal Association – Referral: https://renal.org/information-resources/the-uk-eckd-guide/referral/
- Farrington, K., Rao, R., Gilg, J., Ansell, D., Feest T. New adult patients starting renal replacement therapy in the UK in 2005 (chapter 3) Nephrol Dial Transplant (2007). 22(7): 11–29
- Swidler, M. A. Geriatric renal palliative care. J Gernontol A Biol Sci Med Sci (2012). 67(12): 1400–1409
- United States Renal Data Systems Annual Data Report. 2008
- Farrington, K., Warwick, G. Planning, initiating and withdrawal of renal replacement therapy. UK Renal Association (2009); http://www.renal.org/docs/default-source/guidelines-resources/RRT_-_Current_version__17_September_2009_FINAL.pdf?sfvrsn=0
- Murtagh, F., Cohen, L. M., Germain, M. J. Dialysis discontinuation: quo vadis? Adv Chronic Kidney Dis(2007) 14:379–401
- Wong, C. F., McCarthy, M., Howse, M. L., Williams, P. S. Factors affecting survival in advanced chronic kidney disease patients who choose not to receive dialysis. Ren Fail (2007) 29:653–59
- Hussain, J. A., Mooney, A., Russon, L. Comparison of survival analysis and palliative care involvement in patients aged over 70 years choosing conservative management or renal replacement therapy in advanced chronic kidney disease. Palliat Med (2013) 27(9): 829–39
- Li, H., Xie, L., Yang, J., Pang, X. Symptom burden amongst patients suffering from end-stage renal disease and receiving dialysis: A literature review. Int J Nurs Sci (2018) 5(4): 427-431
- Saini, T., Murtagh, F.E., Dupont, P.J., McKinnon, P.M., Hatfield, P., Saunders, Y. Comparative pilot study of symptoms and quality of life in cancer patients and patients with end stage renal disease. Palliat Med (2006) 20(6):631–636
- Cherukuri, A., Bhandari, S. Analysis of risk factors for mortality of incident patients commencing dialysis in East Yorkshire, UK. QJM (2009) 103(1): 41-48
- Foley, R. N., Parfrey, P.S., Sarnak, M.J: Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis (1998) 32:112-119
- Nolan, C. R. Strategies for improving long-term survival in patients with ESRD. JASN (2005) 16(11): 120-127
