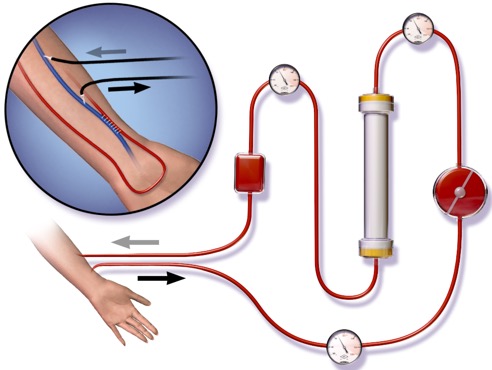
Roughly 30 000 people are receiving haemodialysis (HD) in the UK and 300 people per million population require maintenance HD for end stage kidney disease [1]. Although HD prevents death from renal failure it’s not an infallible treatment….survival after 1 year of HD is about 88% and this drops to about 57% at 3 years [2]. BUT…this will improve to 85% (at 3 years) with transplantation. Quite a few of these patients get transplanted and some that may even pleasantly surprise you! In summary….we know our HD patients very well and want to know when they’re in hospital! We will often oversee their management and can provide advice but here are some top tips to help you master the principles when these patients come to your ward!
So, when will I come across HD patients?
- Two of the main causes of death in dialysis patients are CARDIAC (50% of total mortality) and INFECTION (20%) [3].
- HD patients often have renal failure due to hypertension and diabetes…but add on the burden of inflammation, oxidative stress and hyperparathyroidism and there’s no surprise that cardiac risk is high…
- HD patients often have diabetes, significant uraemia and venous catheters in addition to often having to take immunosuppressants ALL which increase infection risk
- As a result…they have frequent admissions to A&E, the acute medical wards and ITU with sepsis and cardiology with MIs and heart failure
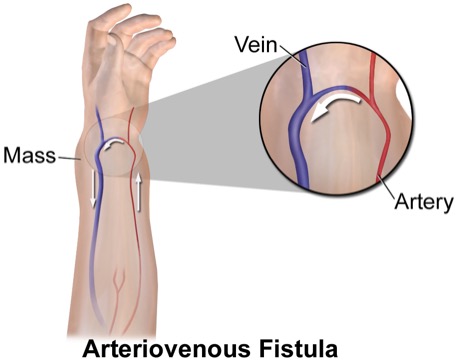
- To add to this….HD patients frequently get complications relating to their access – clotted fistulas and lines, fistula stenosis/aneurysms and even rupture. Endocarditis is seen fairly frequently often related to infected neck lines…so these patients are well known to interventional radiologists and surgeons
- Dialysis is tough…compliance can be an issue as is under-dialysis, electrolyte and fluid complications – all of which present to both renal wards and medicine
What about levels of care for these patients? Is it different?
- When HD patients are unwell, they can get sick very quickly. The good news is that they are frequently reviewed by the renal team so usually have an established treatment escalation plan
- Check with their renal consultant about levels or care and DNAR forms (if in place)
- Levels of care may be surprising given the relatively poor prognosis on dialysis however, for some, HD is a bridge to transplantation and would likely be appropriate for level 2/3 care given this….and…..some patients survive on HD for decades so assumptions cannot be made in this patient population
- Sometimes patients may present to peripheral hospitals (without HD capability) grossly fluid overloaded or hyperkalaemic and may be too sick to transfer to be dialysed on their usual unit….on these occasions, they will probably only be stabilised in ITU and may need a temporary venous catheter for CVVH if they have an AV fistula for access (they can be transferred to their renal/HD centre later)
- BIGGEST TIP: If you have an HD patient on your ward – please let the renal team know as we can help and we may need to adjust aspects of their HD if they are sick/bleeding/due surgery etc. that if we don’t know about could potentially make things worse! Maintenance HD is an outpatient treatment and their HD unit is not usually a place for a sick HD patient
What about Resuscitation?
- HD patients have an increased risk of arrhythmias secondary to electrolyte disturbances and are also vulnerable to circulatory collapse due to sepsis, volume depletion, cardiac tamponade from pericardial effusions
- Follow the Resuscitation Council Guidelines as you would for any other patient [5]
- Here are some TOP TIPS to consider:
- Avoid needling the AV fistula arm for bloods/ABGs and cannulas – their AV fistula really is the patient’s lifeline (morbidity and mortality increases with each loss of access)
- Venous dialysis catheters should not be used for anything other than dialysis UNLESS in extreme circumstances where other access cannot be gained in an emergency scenario
- In haemorrhage scenarios – Desmopressin may be considered to combat uraemic platelet dysfunction (BUT discuss with renal 1st)
- HD patients cannot eliminate water and electrolytes from their body (often even if they still pass a bit of urine) so remember any fluid you give will risk pulmonary oedema
- If fluid really does need to be given – give small boluses and reassess after each
- Check a patient’s usual BP with their dialysis unit – this will really help you with a fluid balance assessment
- Lying-standing (or sitting-lying) BPs will give a good indication of volume depletion (if drop >20/10 mmHg) – as long as no autonomic neuropathy!
- DO NOT use urine output as an indicator of illness/fluid assessment – it is not at all accurate in these patients!
I’ve heard that fluid and electrolyte imbalances are common….
- The main question to ask yourself is….does this patient need dialysis NOW?….all you need to remember are your vowels…..AEIOU
- Acidosis – if serum bicarbonate is <16mmol/L this is considered significant
- Electrolytes – If K+ high – especially if >6.5 with or without ECG changes
- Ingestion (not usually relevant here unless a toxicology patient)
- Overload (volume) – pulmonary oedema
- Uraemia – encephalopathy or pericarditis (you will hear a rub) caused by high urea
- So…acidosis…
- Don’t assume it’s a renal failure acidosis – could it be lactic acidosis from sepsis or ischaemia? DKA? Poisoning? – check the anion gap, lactate, glucose, ketones and take a good history and examination
- What about hyperkalaemia then…?
- If the patient’s normal HD session is due then a K+<6 mmol/L is not very concerning. If their next HD is due in >24 hours then closely monitor the K+. If K+ is >6.5 then put on a cardiac monitor and the patient will have to have dialysis urgently (arrange with renal/ITU)
- Again, don’t assume the high K+ is due to renal failure – other common reasons may be drugs, non-compliance with HD or their low K+ diet, other causes of metabolic acidosis and haemolysis/rhabdomyolysis
- Do not transfer a patient from your hospital to the patient’s HD unit without calling the renal team first if their K+ is especially high – we will assess the risks and help to make alternative arrangements if necessary
- Potassium hiding therapies (e.g. insulin-dextrose) are not typically effective in HD patients – they will need dialysis to lower their K and the underlying cause of high K+ to be dealt with
- After HD, some patients may appear to have low K+ on their post-dialysis bloods – this usually rebounds quickly. It may mean that we need to adjust their dialysis prescription but please do not replace this with oral or IV K+ without discussing with the renal team first
- Pulmonary oedema….?
- HD patients develop pulmonary oedema for a number of reasons:
- Too much fluid in (drinking too much or overzealous IV fluid) or not enough fluid out(missed HD sessions, under-dialysis)
- Heart failure (e.g. due to MIs, diastolic dysfunction from hypertension/LVH)
- Renal artery stenosis (rare though)
- Ultimately, acute coronary syndrome must be ruled out
- Loop diuretics may have a small effect if the patient still has some residual renal function and passes a reasonable amount of urine
- IV nitrates can be used if BP allows
- CPAP will also work as it does in other patients
- HD patients develop pulmonary oedema for a number of reasons:

- And finally…uraemia…
- Typical uraemic symptoms include, nausea, vomiting, anorexia, itch, malaise but severe complications include pericarditis and encephalopathy
- If pericarditic – a pericardial rub is usually heard but not always if there’s a pericardial effusion (check for raised JVP, kussmaul’s sign, muffled heart sounds and pulsus paradoxus AND check an ECG – saddle-shaped ST depression, low amplitude complexes, electrical alterans)
- Remember to avoid anticoagulation if very uraemic as bleeding into the inflamed pericardium can be fatal (r/v once uraemia resolves)
- Remember – encephalopathy may not be due to urea – consider hypoglycaemia, sepsis, drug intoxication, intracranial events and hypertensive emergencies
We will cover more specifically…. ACS, infection, drugs, bleeding and other medical problems in HD in part 2!
References
- UK Renal Registry Annual Report, 2017
- United States Renal Data System, 2017
- Levy, J., Brown, E., Lawrence, A. Oxford Handbook of Dialysis. 4th Edition. 2006, Oxford University Press, Oxford
- https://commons.wikimedia.org/wiki/File:Blausen_0313_Dialysis.png
- Resuscitation Council Guidelines. Resuscitation Council (UK), 2020
- https://commons.wikimedia.org/wiki/File:Blausen_0049_ArteriovenousFistula.png
- https://en.wikipedia.org/wiki/Kerley_lines#/media/File:Chest_radiograph_of_a_lung_with_Kerley_B_lines_-_annotated.jpg