Every junior doctor’s nightmare is the patient with high potassium (K+)! Many calls to the renal registrar occur after a patient has received various numbers of insulin-dextrose infusions and I can guarantee the reason a patient has hyperkalaemia can be quickly identified and fixed. Management of high K+ is believe it or not very straightforward but must be taken seriously…..
First of all…why do we care?
- Well…a retrospective analysis of 932 hospitalised adults in Korea showed that 35.2% of patients with a serum K+ >6.5 suffered arrhythmias and 43.3% had a cardiac arrest [1]
- Incident high K+ predicted mortality at the time of ITU admission….and….even if low level high K+ didn’t correct by 1.0 >meq/L within 48 hours then this continued to predict death [2]
- Interestingly…these studies suggested that it was the velocity and duration of the high K+ as well as the absolute level that predicted mortality
- Reports of acute high K+ causing cardiac arrest typically involve [3]:
- IV K+ loading
- Massive cell turnover
- Shift in K+ during surgical anaesthesia or critical illness
- The K+ was typically normal shortly beforehand and rapidly rose. Remember…this situation is uncommon in humans and is usually incidental and asymptomatic
- The most important thing from these studies is that it wasn’t the high K+ that necessarily caused death…the high K+ was simply a marker of bad news
When should I worry?
- Peaked T waves, prolonged PR interval, flattened p waves, slurring of the ST segment and broad QRS complex can precede the ominous sine wave pattern on the ECG in high K+
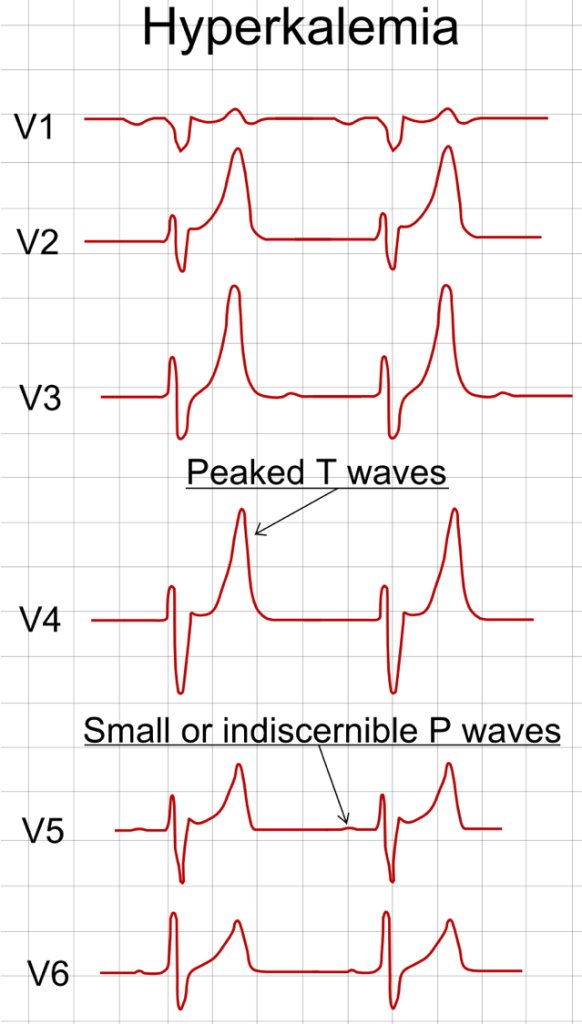
- AND….high K+ predisposes to both cardiac hyperexcitability (VT and VF) and cardiac depression (bradycardia, AV block, intraventricular conduction delay and asystole)
- BUT….most reports show that there is a large degree of disconnect between severity of high K+ and expected ECG findings
- Studies suggest that BRADYCARDIA, JUNCTIONAL RHYTHMS and QRS WIDENING are associated with adverse outcomes
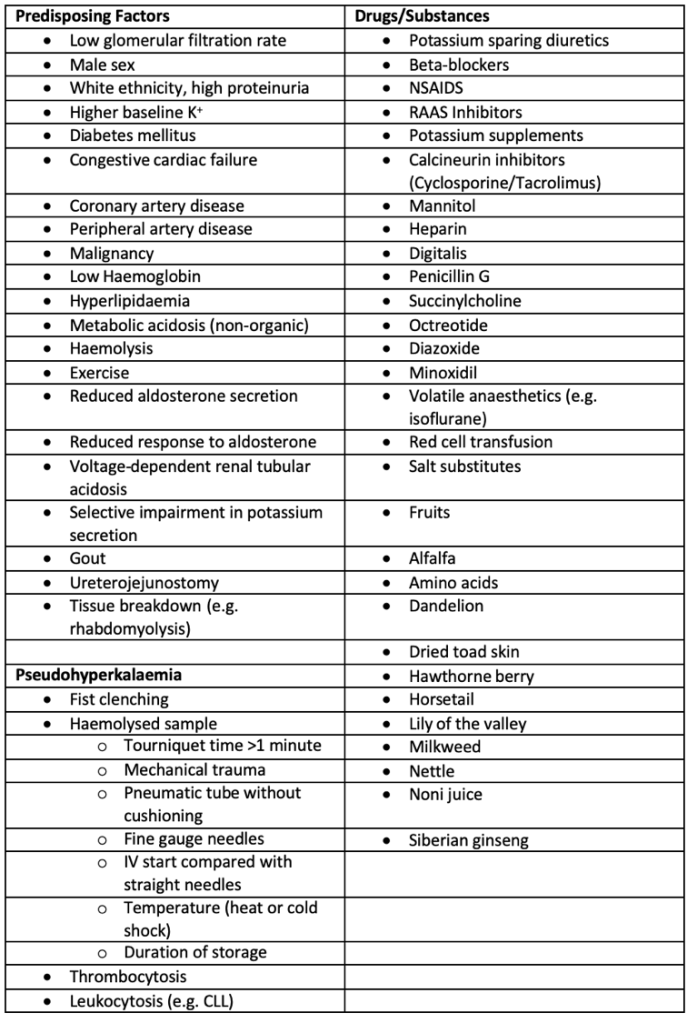
- Based on this…KDIGO guidance suggests classifying high K+ severity based on the table below:
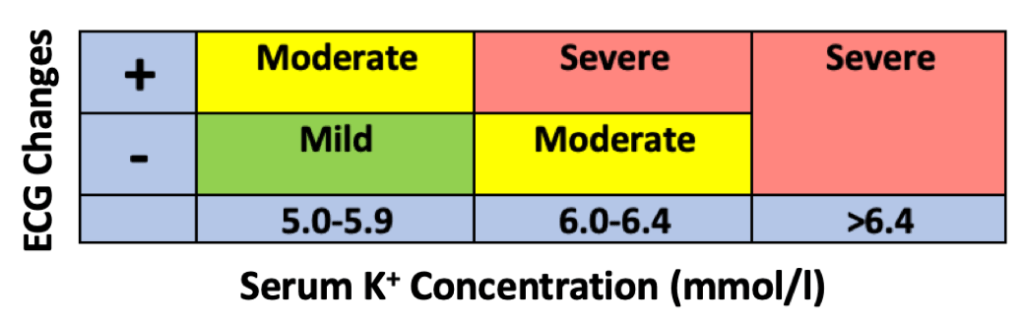
- BUT…normal ECGs have been seen in patients with severe chronic hyperkalaemia so…in summary…..we don’t know how sensitive they are at predicting death from high K+
- Many U-shaped curves have shown the relationship between high and low K+ with mortality [5]
Is it actually high?
- Lets talk about pseudohyperkalaemia….a falsely higher K+ in serum compared to plasma – this is due to:
- Haemolysis (haemolytic conditions, small gage venesection needle, tourniquet use >1 minute, blood clotting, mechanical trauma, fist clenching during venesection, high temperature in tube or body, long storage)
- Cell fragility
- Heparin-induced damage
- Myeloproliferative disorders
- Thrombocytosis
- But have you heard of REVERSE pseudohyperkalaemia…? This a falsely high K+ in plasma compared to serum – this is due to:
- Haematologic malignancy
- Heparin-induced cell membrane damage (during processing or mechanical damage during lab transport)
- So….how to you get a genuine K+ then??…..if a repeat sample doesn’t help – do a VBG
What do I do?
- Repeat the sample
- If you suspect pseudohyperkalaemia – look at FBC, consider haemolysis and if suspected then do a haemolysis screen and do a VBG
- Perform an ECG
- Review drugs…any that may cause high K+?
- Check renal function….Is there a reason that K elimination might not be working i.e. in CKD/AKI
- If CKD or AKI….check dietary potassium intake and check urine output
- In very rare cases the patient might have a genetic condition that causes high K+ – check the notes for this (the high K+ will still need to be taken seriously though)
How do I treat it?
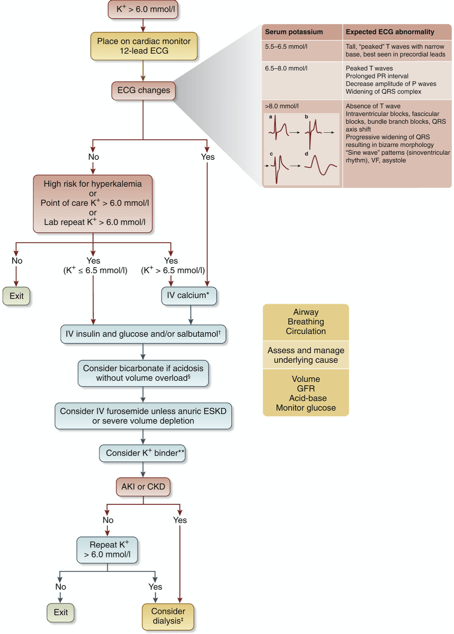
[6]
- Here is what KDIGO recommend, however, you must follow your own local hyperkalaemia protocol….but we shall share some pearls…
- Clinical pearls from our experience….:
- The high K+ will continue to rebound with treatment unless you identify and fix the underlying cause
- Patients with ECG changes should be put on a cardiac monitor
- The management of outpatients and high K+ is a different ballgame…
- Only send to A+E if severe high K or unwell
- Stop or reduce ACEi/ARB (or other K sparing drugs)
- Arrange repeat
- Low K diet sheet
- Can add loop or thiazide diuretic (if not dry) or fludrocortisone (if not overloaded or cardiac disease as there are big benefits for blocking aldosterone in HF)
- Remember to carefully outline a ACEi/ARB re-initiation plan – stopping these drugs in cardiac patients is akin to stopping chemotherapy!
- IV calcium (gluconate or chloride):
- Does not reduce the K+…it buys you time by stabilising the heart
- Only has a short duration of action (minutes)
- Subsequent doses should be given if ECG changes persist for >5 minutes
- Chloride contains more calcium than gluconate
- Gluconate is preferred to chloride as chloride can cause tissue necrosis
- Salbutamol nebulisers:
- The dose is considerably bigger than used for asthma/COPD i.e. 10-20mg
- High rate of AEs – tachycardia, tremor, anxiety symptoms
- Supresses the K+ at a peak of 120 mins after use (90 mins in 20mg)
- As it’s a potassium hiding therapy – K+ will rebound after treatment
- Insulin-dextrose:
- This is a K+ hiding therapy only – it doesn’t lower the total body amount
- K+ will also rebound after this treatment so fix underlying cause
- This treatment is not without risk – deaths have occurred due to hypoglycaemia so…..use cautiously and monitor blood sugar carefully
- Bicarbonate:
- 1.26% IV (isotonic) should only be used as an adjunct to other treatments, not alone and only if acidosis is normal anion gap secondary to AKI
- Although no evidence actually exists…it is thought to cause volume overload so don’t give in very oedematous patients
- Don’t give in rhabdomyolysis (can cause muscle CaPO4 deposition), hypocalcaemia (will worsen) and in patients with low GCS or airways disease (as they are unable to raise their respiratory rate to blow off the excess CO2 so it will accumulate and worsen acidosis) – it can be life threatening in these scenarios
- 8.4% IV (hypertonic) can cause such a big osmolar drag of K+ into the extracellular space that it may outweigh the correction of acidosis to reduce K+
- Potassium binders:
- Lack of evidence in the acute setting
- Cause severe constipation (prescribe with laxatives ++) and in some cases bowel wall necrosis
But what about the underlying cause…?
Which UK guidelines will help?
- Your local hyperkalaemia protocol is where you should start
- If you feel out of your depth or suspect that we need to be involved then call the renal team
- KDIGO
- Renal Association
- NICE
- National Kidney Foundation
References
- An, J. N. et al. Severe hyperkalemia requiring hospitalization: Predictors of mortality. Crit Care 2012, 16: R225
- McMahon, G. M., Mendu, M.L., Gibbons, F.K., Christopher, K.B. Association between hyperkalemia at critical care initiation and mortality. Intensive Care Med 2012, 38: 1834-1842
- Montford, J. R., Linas, S. How Dangerous Is Hyperkalaemia? J Am Soc Nephrol 2017, 28(11): 3155-3165
- https://commons.wikimedia.org/wiki/File:ECG_in_hyperkalemia.png
- Conway, R., Creagh, D., Bryne, D. G., O’Riordan, D., Silke, B. Serum potassium levels as an outcome determinant in acute medical admissions. Clin Med 2015, 15(3): 239
- Clase, C. M. et al. Potassium homeostasis and management of dyskalaemia in kidney diseases: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kid Int 2020, 97(1): 42-61